Continued from my last post...
Apparently, my closest friends had noticed my unending depression, so like all concerned girlfriends, they talked amongst themselves. A LOT of them were in on the discussion, it seems - at least six that I know of, so far - and they also conferred with my husband about how I always seemed tired, hardly left the house, didn't socialize much, looked like crap and so on. Essentially, they felt that I was "stuck" and needed help - professional help - to move forward.
And so, one girlfriend called to say that she'd be near my home Friday morning and wanted to stop by for a quick visit. "Sounds good," I said. "Looking forward to seeing you."
On her way to my place Cari called to tell me that she would arrive soon. "By the way, Carolyn is stopping by, too," she said.
Wow, I thought,
This is great. It's going to be fun to catch up. I'm so gullible sometimes. Duh. It's Friday morning and two of the busiest people I know are skipping work to "pop in and for a quick visit." Yeah, right.
The gals arrived and with coffee mugs in hand, we settled into the living room and chit-chat ensued. Within a couple of minutes, though, the conversation turned serious. They told me how they had observed my blues, the rut I was in, the considerable duration of my depression. Carolyn and Cari confessed that they had spoken to others, including my husband. They explained their wish for me to work through my depression, and their belief that I needed professional help to do so. They told me about a good counseling resource that accepted my medical insurance and offered a few names.
After a few silent moments of pondering, I had to agree with them.
I needed professional counseling to help me through my depression. The cost was a concern (we are BROKE!), but I pledged to make the necessary phone calls and obtain the assistance I needed.
 A brief aside about friends:
A brief aside about friends: I often think about my friends and how much I value them. As stated on a needlepoint piece that was a gift from a girlfriend, "Friends are the family you choose."
My friends truly are my family, because outside of my husband and children, they are my primary sources of encouragement and emotional support. Regardless of the need, I can always find friends' helping hands reaching my way. And if the need is extreme, my friends band together and "circle the wagons," as they did during my transplant.
My closest friends also love me enough to intervene, sit me down and tell me the harsh truth, even though it might hurt me to hear it. Not just anyone can get away with that. And there aren't many people I love and trust enough to hear clearly, even when the news is bad. Each of these friends is worth her weight in gold.
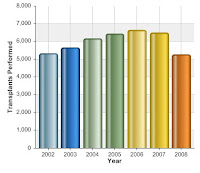
So I did as promised. It took about three weeks altogether, but I received authorization from our health insurance company, made an appointment and finally met with a counselor just before Christmas. I'll tell you about the appointment and about a long, difficult conversation with my husband - which proved to be my "Eureka!" moment - in another post. My next post is going to address transplants and depression, and some of the things I've learned about this issue and how it is - or isn't - managed through the healthcare system.
 liver transplant. What a wonderful occasion! There have been plenty of times when I wondered if I'd make it this far, so celebrating the day is a blessing.
liver transplant. What a wonderful occasion! There have been plenty of times when I wondered if I'd make it this far, so celebrating the day is a blessing.